A new study shows a bidirectional relationship between COVID-19 diagnosis and the risk of developing a psychological illness
In a cohort study recently published in Lancet Psychiatry, researchers set out to determine whether a COVID-19 diagnosis increased the risk of diagnosis with subsequent psychiatric illness (primarily anxiety, depression, dementia, and insomnia) in weeks shortly thereafter. Additionally, the researchers evaluated whether or not having a psychiatric illness increased the risk of contracting COVID-19. The results they found were astonishing.
There has been much concern over the lasting psychological sequelae as a result of contracting COVID-19. Until recently, the documented effects of coronavirus on mental health and on patients with mental illness have been limited. Several studies have investigated the impact of COVID-19 on mental health but only through anecdotal evidence via surveys and self-reported symptom questionnaires. To date, none have looked at official psychiatric diagnosis as a result of COVID-19 making this a novel study with clinically applicable findings.
The study used an electronic health record database from 54 health-care organizations across the United States and selected approximately 62,000 individuals diagnosed with COVID-19 between Jan 20, 2020 (date of first recorded COVID-19 case in the U.S.) and Aug 1, 2020, for the cohort. Of these cases, approximately 73% had no previous mental health diagnosis and were compared to control groups hospitalized for conditions independent of COVID-19 (i.e. influenza, other respiratory tract infections, skin infections, cholelithiasis, urolithiasis, and fracture). Confounding variables such as predisposing conditions and behavioral risk factors were accounted for and factored into the statistical analysis of the study results.
The primary outcome of this study, diagnosed with a psychiatric illness 14 to 90 days after being diagnosed with COVID-19, showed a 58% to 224% increased likelihood of the first-time diagnosis with a psychiatric illness compared to controls. Furthermore, the estimated probability of diagnosis with a psychiatric illness after COVID-19 was 5.8% after 90 days post-diagnosis with the most common diagnosis being anxiety disorders (adjustment disorder, generalized anxiety disorder, PTSD, and panic disorder) at 12.8% followed by mood disorders (9.9%).
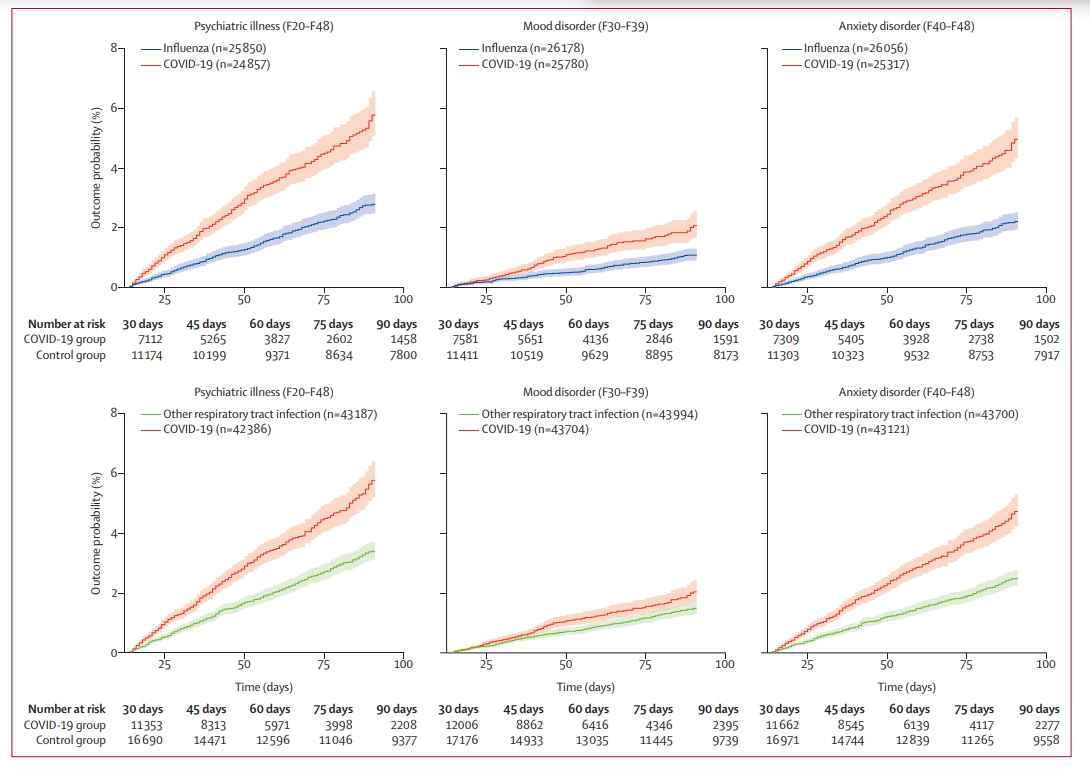
Figure 1- Curves represent the onset of first psychiatric diagnosis 14 to 90 days after being diagnosed with COVID-19 compared to control groups diagnosed with other respiratory tract infections1.
Results indicated a low probability of psychotic disorder diagnosis in the 14 to 90 days after COVID-19 diagnosis (0.1%) similar to control groups without COVID-19 diagnosis. The rate of first or relapsed psychotic disorder was 0.9% which was significantly higher than controls. The probability of insomnia diagnosis was significantly higher in the COVID group than in control groups at 1.9% and the probability of being diagnosed with dementia in adults 65 years of age or older was 1.6%, more than double the control group. The probability of being diagnosed with any psychiatric illness in the 14 to 90 days after COVID-19 diagnosis was 18.1% compared to controls and those requiring in-patient admission for COVID-19 treatment were at a 40% higher risk of psychological sequelae.
Of note, the control group had higher rates of psychiatric sequelae when health events occurred on or after April 1, 2020, and the differences in outcome between control groups and COVID-19 diagnosed patients were less substantial. Nonetheless, the rate of psychiatric illness was still higher after contracting the coronavirus.
Furthermore, having a psychiatric disorder diagnosis in the year prior to the global pandemic was associated with a 65% increased risk of contracting COVID-19 and was highest in older patients. The results remained significant if it was the patient’s first psychiatric diagnosis, were diagnosed in the past 3 years, among patients whose race was known, no physical risk factors for COVID-19, and problems related to housing or economic circumstances. There was no major difference between the risk of the coronavirus when comparing psychiatric diagnoses against each other.
Based on these findings we can infer that patients diagnosed with COVID-19 have an increased risk for mental illness or symptoms of psychological sequelae in the weeks following coronavirus. It is difficult to say whether this is attributed to the impact of the virus directly or the psychological distress that comes with contracting an infection we still don’t know much about. However, it is safe to assume that the coronavirus impacts mental health, and those already diagnosed with psychiatric illness are at an increased risk for contracting the virus.
If you would like more information about therapy treatment services, please contact Specialized Therapy Associates at (201)-488-6678 to make an appointment. You can also visit us online at Specialized Therapy.
By Taylor Groff, MS Functional Nutritionist
References:
- Taquet, M., Luciano, S., Geddes, J.R., Harrison, P. (2020). Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62,354 COVID-19 cases in the USA. The Lancet Psychiatry. DOI:https://doi.org/10.1016/S2215-0366(20)30462-4.

