The Power of the Vagus Nerve in Healing Trauma
Lizzie Delfeld
Tags: Vagus Nerve, Trauma, Healing, Nervous System
Do you ever feel stuck?
Do you ever feel like, no matter how hard you try, you always find yourself in similar problem situations?
Maybe you just can’t help but get angry at the car that cuts you off, or you just can’t stand it when your partner is late (as always). Maybe you can’t open yourself up to people, no matter how hard you’ve tried to change your ways. Or, maybe there are certain situations that always bring forth protective and generally unpleasant reactions within you?
Whatever it may be, there is new research that might explain why. A new theory concerning the vagus nerve, and its effect on our nervous system, might help explain why we are hardwired into certain patterns or habits.
The Vagus Nerve
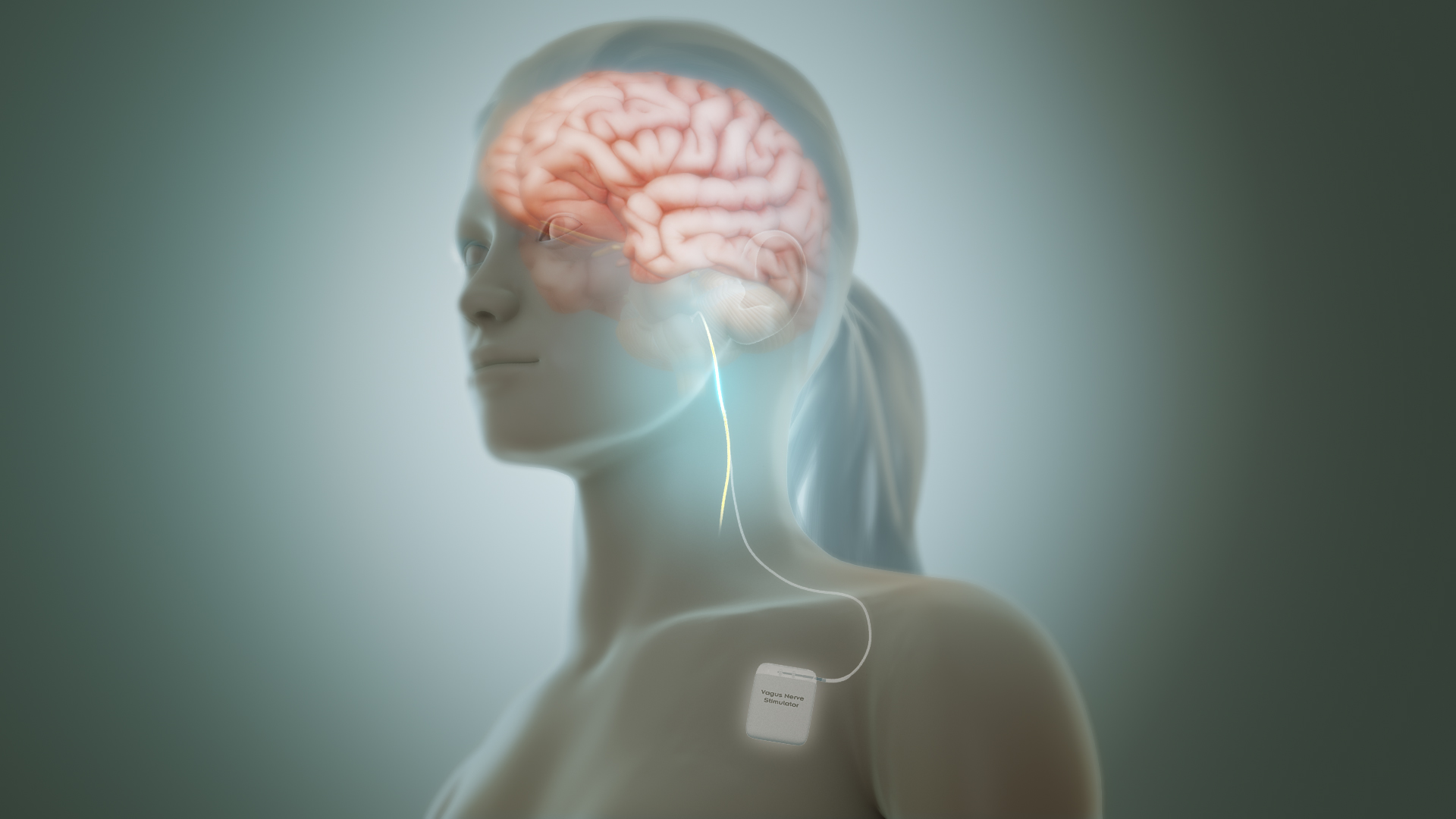
The vagus nerve is the longest cranial nerve in our body, considered a part of the parasympathetic nervous system (i.e. the part of the nervous system responsible for calming the body down, after the sympathetic nervous system activates it for whatever reason).
This nerve is found in most vertebrates, and is made up of both sensory and motor fibers. It’s primary purpose is to connect various organs to the brain, and notably, it connects the brain to the enteric nervous system, the collection of nerves connected to the intestines and digestive system, also known as the “gut brain.”
It is, in essence, the mind-body connection point, and as of late, there is much energy and conversation around how studying this nerve and its relation to other body systems can help improve and alleviate the symptoms of both mental and physical illness.
Vagal Tone
One element that has garnered much attention is the concept of one’s vagal “tone.” A high vagal tone, one in which the nerve activates more readily when faced with stimuli, results in low inflammation, higher ability to regulate emotions, and a strengthened immune system, among other things.
By working to activate this central nerve, various times a day, the idea is one can increase their vagal tone. In this way, the vagal nerve becomes used to being activated, and might not invoke such dramatic responses in the individual when faced with a triggering stimulus. Additionally, this theory purports that a higher vagal tone can perhaps also reduce some of the deleterious effects that chronic stress, in whatever form we experience it, has on our body systems. So, this might be one of the reasons you are seeing so many people trying out deep breathing exercises, or others raving about their new cold shower or ice bath routines. Of course, other practices, like exercise, meditation, and even singing/humming are other ways one can easily stimulate this very central and important nerve.[2] Polyvagal Theory In the past, the field of bioelectronic medicine has been able to help treat people with conditions rheumatoid arthritis, epilepsy, and severe depression by implanting an electrode into patients to stimulate the vagus nerve[3]. However, in recent years Dr. Stephen Porges has opened our understanding of the importance of this nerve in an even more nuanced way, with his development of polyvagal theory. There are two vagal circuits of the parasympathetic nervous system. The first, the central vagal complex, or the “social nervous system,” is activated when we find connection in our environment, and works to soothe our bodily stress response[4]. The other, a more primitive system called the dorsal vagal complex, is evolutionarily much older than the social nervous system, and much slower to activate and deactivate. When we are in distress, and the sympathetic nervous system has ramped up, our body’s first response is to first use this social nervous system — looking to things in our environment to return us to a sense of relative safety. However, when this approach fails for whatever reason, the older dorsal vagal complex activates, this alternate response slows our bodily functioning, and mobilizing defensive strategies like dissociation or, in some cases, fainting.[5] This theory has helped to, in part, explain why dissociation and disconnection may occur for individuals with histories of trauma. When utilizing this dorsal vagal response is routinely used, it becomes a more ingrained nervous system response, thus making it more difficult to activate the alternative, central vagal complex response. This dorsal vagal response of the vagus nerve sits in the nervous system of reptiles, showing it’s primitive nature. And in terms of the time it takes to activate and deactivate, it unfortunately is a much slower response, making it arguably not as adaptive to the pressures and demands of the nuanced and fast-paced modern world we live in. However, we do still use this dorsal vagal response at times. Important to note is that, once in this dorsal vagal mode of functioning, it is much more difficult to switch over and reactivate the social/environmental coping abilities of the “social nervous system.” — The potential that this new information has on the future of treatment of PTSD is great. Additionally, polyvagal theory and new treatments designed from this framework of thinking could also potentially help treat conditions such as irritable bowel syndrome or chronic depression, in addition to PTSD, as the vagus nerve is intimately tied to our gut brain. If you or anyone you know may have mental, emotional or physical concerns please contact Specialized Therapy Associates at 201-488-6678 or The Functional Medicine Center for Personalized Care, LLC (www.FxMedCenters.com) at 201-880-8247 where an intake coordinator will provide answers to any of your questions and connect you with the professional who is right for you. [1] Arielle Schwartz, “Natural Vagus Nerve Stimulation,” Arielle Schwartz PhD, 7/19/2015, https://drarielleschwartz.com/natural-vagus-nerve-stimulation-dr-arielle-schwartz/#.YJqrnJNKjBJ. [2] Fallis, Jordan. “How to stimulate your vagus nerve for better health.” Jordan Fallis. 1/21/2017. https://sass.uottawa.ca/sites/sass.uottawa.ca/files/how_to_stimulate_your_vagus_nerve_for_better_mental_health_1.pdf [3] Arielle Schwartz, “Polyvagal Theory Helps Unlock Symptoms of PTSD,” Arielle Schwartz PhD, 7/19/2015, https://drarielleschwartz.com/polyvagal-theory-unlocks-symptoms-of-ptsd-dr-arielle-schwartz/#.YJrI_5NKjBI. [4] Arielle Schwartz, “Polyvagal Theory Helps Unlock Symptoms of PTSD,” Arielle Schwartz PhD, 7/19/2015, https://drarielleschwartz.com/polyvagal-theory-unlocks-symptoms-of-ptsd-dr-arielle-schwartz/#.YJrI_5NKjBI. [5] Arielle Schwartz, “Polyvagal Theory Helps Unlock Symptoms of PTSD,” Arielle Schwartz PhD, 7/19/2015, https://drarielleschwartz.com/polyvagal-theory-unlocks-symptoms-of-ptsd-dr-arielle-schwartz/#.YJrI_5NKjBI.
By treating and respecting the mind and body connection, we are creating new avenues to become unstuck. If you have a history of trauma, depression, or have symptoms in the brain, gut or general health, I encourage you to dive into the new research literature about the polyvagal theory and its potential to rewire our unconscious, automatic nervous system responses. Our specialists will help you improve vagal tone and remit symptoms.